The Large Intestine and Rectum
The large intestine and rectum are part of the digestive system, characterized as a long tube with muscular walls, about 5-8 centimeters in diameter and approximately 6 feet long. Their function is to absorb water from ingested food and store waste before it is excreted from the body through the anus.
Understanding Cancer and Metastasis
Cancer is a disease caused by abnormal cells dividing continuously and uncontrollably, forming a large mass called a "malignant tumor." When cancer enters the bloodstream or lymphatic system and appears in other parts of the body, it is called metastasis.
Colorectal Cancer
Colorectal cancer is a malignancy of the large intestine and rectum tissues. The most common type originates from abnormal changes and growth in the lining cells, forming small growths called polyps. These polyps take time to develop into cancer.Removing the polyp can prevent it from developing into cancer. Untreated colorectal cancer may spread through the intestinal wall or metastasize to the liver, lungs, peritoneum, brain, or bones.
Indicative Symptoms of Colorectal Cancer
The following symptoms are a group of signs that may indicate colorectal cancer:
- Changes in bowel habits: Bowel habits change from the person's normal routine, possibly becoming more frequent or more constipated. This may also include a feeling of incomplete evacuation or straining.
- Alternating diarrhea and constipation.
- Fresh blood or dark red/clotted blood mixed with stool.
- Stool with an abnormal appearance, such as flat, ribbon-like stools.
- Bloating, abdominal pain, discomfort, flatulence, or excessive gas (Abdominal Discomfort).
- Unexplained weight loss.
- Fatigue and weakness, inability to perform normal daily activities.
>> If you experience these symptoms, you should consult a doctor immediately for a physical examination and diagnosis.
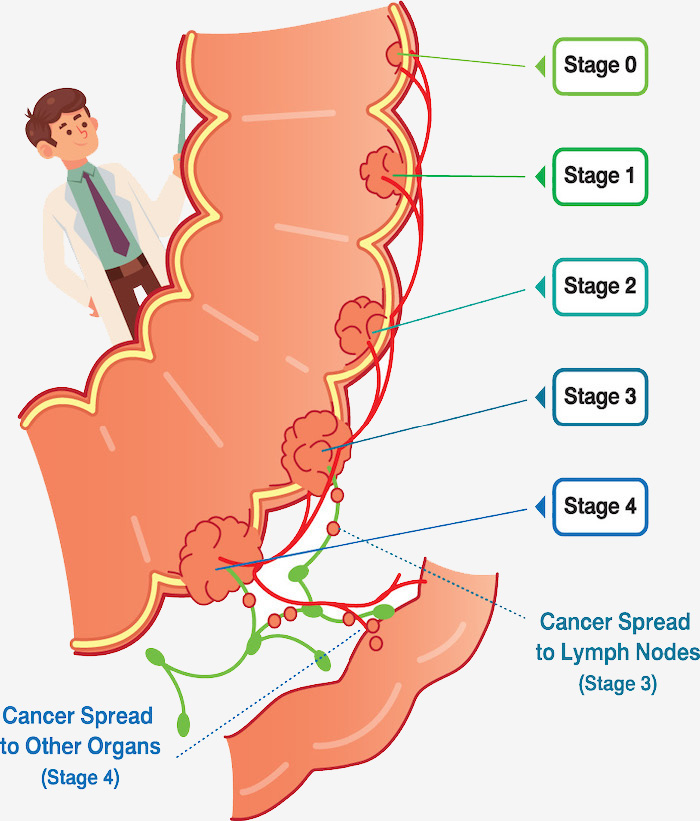
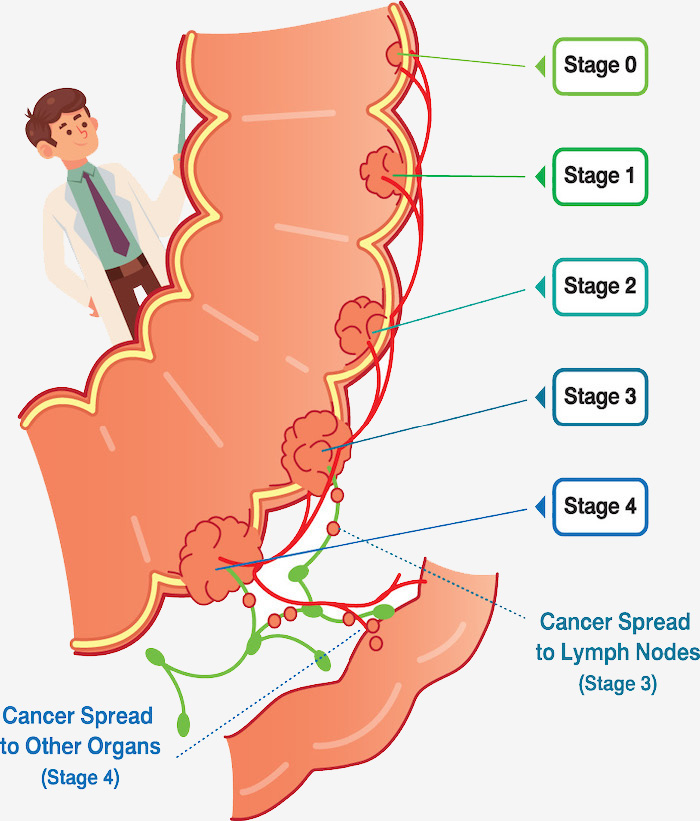
Stages of Colorectal Cancer and Treatment Methods
- Stage 1. Disease Characteristics: The tumor grows larger than stage zero and invades the muscle layer of the large intestine and rectum, but does not spread to adjacent tissue or lymph nodes, and does not penetrate the muscle layer.
Treatment: Surgical removal of the cancerous part of the intestine. - Stage 2. Disease Characteristics: The tumor spreads to the outer wall of the large intestine and rectum or nearby tissues, but has not yet spread to the lymph nodes.
Treatment: Surgical removal of the cancerous intestine. Some cases may require chemotherapy after surgery. For distal colorectal cancer, chemotherapy combined with radiotherapy may be given before or after surgery. - Stage 3. Disease Characteristics: The cancer has spread out of the intestine into the lymph nodes surrounding the large intestine, but has not yet spread to other organ.
Treatment: Surgical removal of the cancerous part of the intestine, combined with chemotherapy after surgery. For distal colorectal cancer, chemotherapy combined with radiotherapy may be given before or after surgery. - Stage 4. Disease Characteristics: The cancer has metastasized to various organs in the body, most often spreading to the liver and lungs.
Treatment: Chemotherapy is administered, and targeted therapy may be considered for improved efficacy. In some patients, surgery may also be included.
Screening for Colorectal Cancer
Screening for the general population without suspicious symptoms aims to detect cancer in its early stages to reduce mortality from the disease. Colorectal cancer screening can be done in several ways:
- Stool-based Test: Two methods:
- Fecal Occult Blood Test (FOBT): Detects red blood cells that may be hidden in the stool, or small amounts of blood (Occult Blood) not visible to the naked eye.
- Fecal DNA Testing: Colorectal tumors shed cells, allowing for the detection of abnormal DNA in the stool.
- Imaging Tests:
- Computed Tomographic (CT) Colonography: An advanced technique involving inflating the large intestine with air to maximize clarity, then performing a cross-sectional X-ray. The data is used to create a three-dimensional virtual image of the colon's interior to detect abnormalities like polyps or other lesions.
- Flexible Sigmoidoscopy: Insertion of a scope through the anus to examine the rectum and flexible colon. If lesions are found, a biopsy can be performed for further investigation.
- Colonoscopy: Insertion of a scope through the anus to visualize the entire rectum and large intestine. This method allows for the removal of suspicious tissue for pathological examination and is the most accurate diagnostic method.
Treatment Guidelines
- Surgery: The primary goal is to remove the tumor from the body. The surgeon removes the cancerous part of the intestine along with nearby lymph nodes. The remaining parts of the intestine are then reconnected. If reconnection is not possible, acolostomy (opening of the large intestine through the abdominal wall) may be created temporarily or permanently, depending on the patient's condition and the extent of cancer invasion. The opening of the large intestine through the abdominal wall changes the direction of waste excretion from the body.
- The opening of the large intestine through the abdominal wall is called a Colostomy.
- Radiation Therapy:
- Uses high-energy radiation to destroy cancer cells. Typically used for patients with rectal cancer.
- Before surgery: To shrink the tumor and simplify the operation.
- After surgery: To destroy any remaining cancer cells and reduce the rate of recurrence.
- Chemotherapy is often combined with radiotherapy to enhance treatment.
Currently, the combination of radiation and chemotherapy in patients with rectal cancer can reduce recurrence and lower the rate of needing a permanent colostomy.
- Chemotherapy:
In patients with very large tumors or cancer spread to the lymph nodes, chemotherapy is usually given after surgery (called adjuvant therapy) to eliminate remaining cancer cells. This treatment is given to reduce the risk of cancer recurrence and improve patient survival. This is called curative treatment. Chemotherapy is also the main treatment for metastatic colorectal cancer or patients unfit for surgery. In this case, chemotherapy is used to stop the spread of cancer, alleviate symptoms or suffering, ensure the best quality of life, and prolong patient survival. This is called palliative treatment.
Two methods of Chemotherapy Administration:- Intravenous Chemotherapy: Administration of chemotherapy by injection is the standard method of treatment. Usually, more than one drug is used in combination for maximum efficacy. Dosing is given in cycles with rest periods, depending on the regimen. The physician will select the most appropriate regimen for each patient.
- Oral Chemotherapy: Has similar efficacy to intravenous chemotherapy. This form was developed to increase convenience for the patient, caregiver, and family, allowing for a more normal life, as intravenous chemotherapy can sometimes cause pain and require time spent at the hospital for administration.
Targeted Therapy:- A new treatment that directly inhibits cancer. Examples include Anti-Angiogenesis Therapy (inhibits new blood vessel formation) and Anti-epidermal growth factor receptor (inhibits cancer growth).
- These drugs are often given in combination with chemotherapy for better efficacy. They have been found to help prolong survival, increase disease-free survival, and improve tumor response rates more than chemotherapy alone. The specialist will recommend which drug is suitable for which patient. It is important to know that the choice of drug can differ among patients because even if they have the same type of cancer, the mutations in the cancer cells may differ. Therefore, testing for cancer cell mutations using Comprehensive Genomic Profiling can help the doctor and patient collaboratively plan the most appropriate treatment and select the best drug.
- Common side effects from targeted therapy include:
- Anti-Angiogenesis drugs: High blood pressure, blood clots, easy bleeding, wound dehiscence, gastric/intestinal perforation, or protein in the urine.
- Anti-epidermal growth factor receptor drugs: Diarrhea, rash, dry/peeling skin, or sun sensitivity.
Follow-up
After treatment, patients are monitored by the treating physician for ongoing health care. Follow-up is typically every 3-6 months for the first 2 years, and every 6 months up to 5 years. Follow-up includes physical examination, cancer marker blood tests, and other tests such as colonoscopy and radiological diagnostics, with the timing determined by the physician.